Dr. Farr Nezhat pioneered the safe treatment of ovarian cysts and adnexal masses of all sizes using minimally invasive surgery (MIS) and has published many peer-reviewed papers on the topic. He’s demonstrated the efficacy of laparoscopy for ovarian cysts and is considered among the best ovarian cysts specialists in the world.
What are ovarian cysts and adnexal masses?
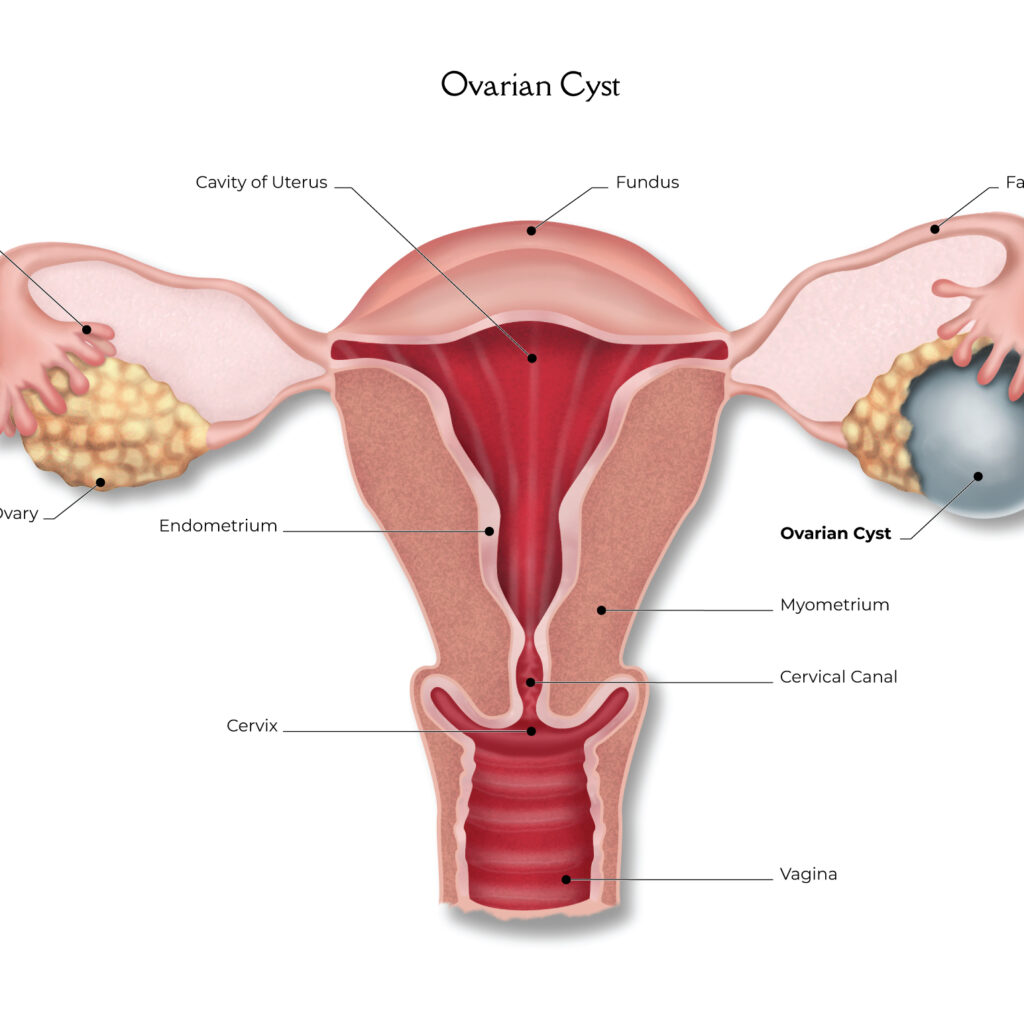
- OVARIAN CYSTS are fluid filled sacs within or on the surface of an ovary. In many cases they are small, harmless, and devoid of symptoms. However, if they are large, rupture, cause the ovary to twist, cause symptoms such as pain or infertility, or are suspicious for cancer, they may require surgical intervention.
- FUNCTIONAL CYSTS are formed during the menstrual cycle and are the most common type. Follicular Cysts form when an egg sac fails to burst and release a mature egg. The sac then grows into a cyst, but these often resolve gradually within a couple months and don’t require treatment. Corpus Luteum Cysts form after an egg sac bursts and releases a mature egg, but the remaining sac fails to shrink away and instead reseals itself and builds up fluid inside. These may grow large, bleed or twist the ovary (restricting blood supply), thereby necessitating treatment.
- ENDOMETRIOTIC CYSTS (ENDOMETRIOMAS) result from endometriosis. Endometrial-like tissue grows outside the uterus, attaches to an ovary, responds to hormonal fluctuations, and accumulates as a cyst. These can cause pain, infertility, and adhesions, and they have the potential to rupture.
- BENIGN NEOPLASTIC CYSTS are not formed as part of the menstrual cycle and can have fluid or solid components. Cystic Teratomas (dermoid cysts) are formed from cells that are present at birth, grow slowly over many years, and do not resolve on their own. They are formed during fetal development and result from entrapped skin structures (hair follicles, sweat glands, hair, teeth, or nerves). Mucinous Cystadenomas contain mucous material and Serous Cystadenomas contain clear yellow fluid. They can both become very large.
- MALIGNANT CYSTS are ovarian cancer, but they are rare. Any cyst may become cancerous, so it is crucial cysts be evaluated and monitored.
Adnexal Masses
The term “adnexal” refers to structures connected or related to the uterus, such as ovaries, fallopian tubes, and connective tissue. Ovarian cysts and uterine fibroids are sub-types of adnexal masses. Other common types of adnexal masses include:
- ECTOPIC PREGNANCY typically occurs in the fallopian tubes, but can occur elsewhere such as in the ovary, abdominal cavity or cervix. It can cause pain, rupture and bleeding.
- TUBO-OVARIAN ABSCESS, which is a pocket of puss resulting from acute infection, or PID (pelvic inflammatory disease), requiring immediate intervention.
Adnexal masses can sometimes cause torsion of the ovary and cut off the blood supply, resulting in pain and possibly impeding ovarian function.
What are symptoms of ovarian cysts and adnexal masses?
- Pelvic pain
- Painful urination
- Bladder dysfunction
- Painful bowel movements
- Bowel dysfunction
- Painful intercourse
- Infertility
What treatment options does Dr. Nezhat offer ovarian cysts and adnexal masses?
Dr. Nezhat specializes in the application of minimally invasive surgical techniques to treat ovarian cysts and adnexal masses. Laparoscopy and robotics are particularly well suited to treating these conditions due to increased magnification and reach of the surgical instruments.
Dr. Nezhat has contributed numerous surgical “firsts” to the medical literature, establishing evidence-based protocols for improved patient care. He demonstrated the ability to manage adnexal masses by laparoscope instead of by laparotomy.
A listing of over 226 of Dr. Nezhat’s research articles can be found at the PubMed search engine, which pulls references and abstracts from the U.S. National Library of Medicine (NLM) database maintained at the National Institutes of Health (NIH).